| ** | Latin American Journal of Clinical Sciences and Medical Technology is an open access magazine. To read all published articles and materials you just need to register Registration is free of charge. Register now If you already have registered please Log In | ** |
aClínica HealthSkin, Mexico City, Mexico; bClínica Inoui, Mexico City, Mexico; cPráctica privada, Mexico City, Mexico.
Corresponding Author: , . Telephone number: ; e-mail: damarin.rivera@gmail.com
Lat Am J Clin Sci Med Technol. 2025 Nov;7:100-105.
Received: September 23rd, 2025.
Accepted: October 27th, 2025.
Published: November 14th, 2025.
Views: 1562
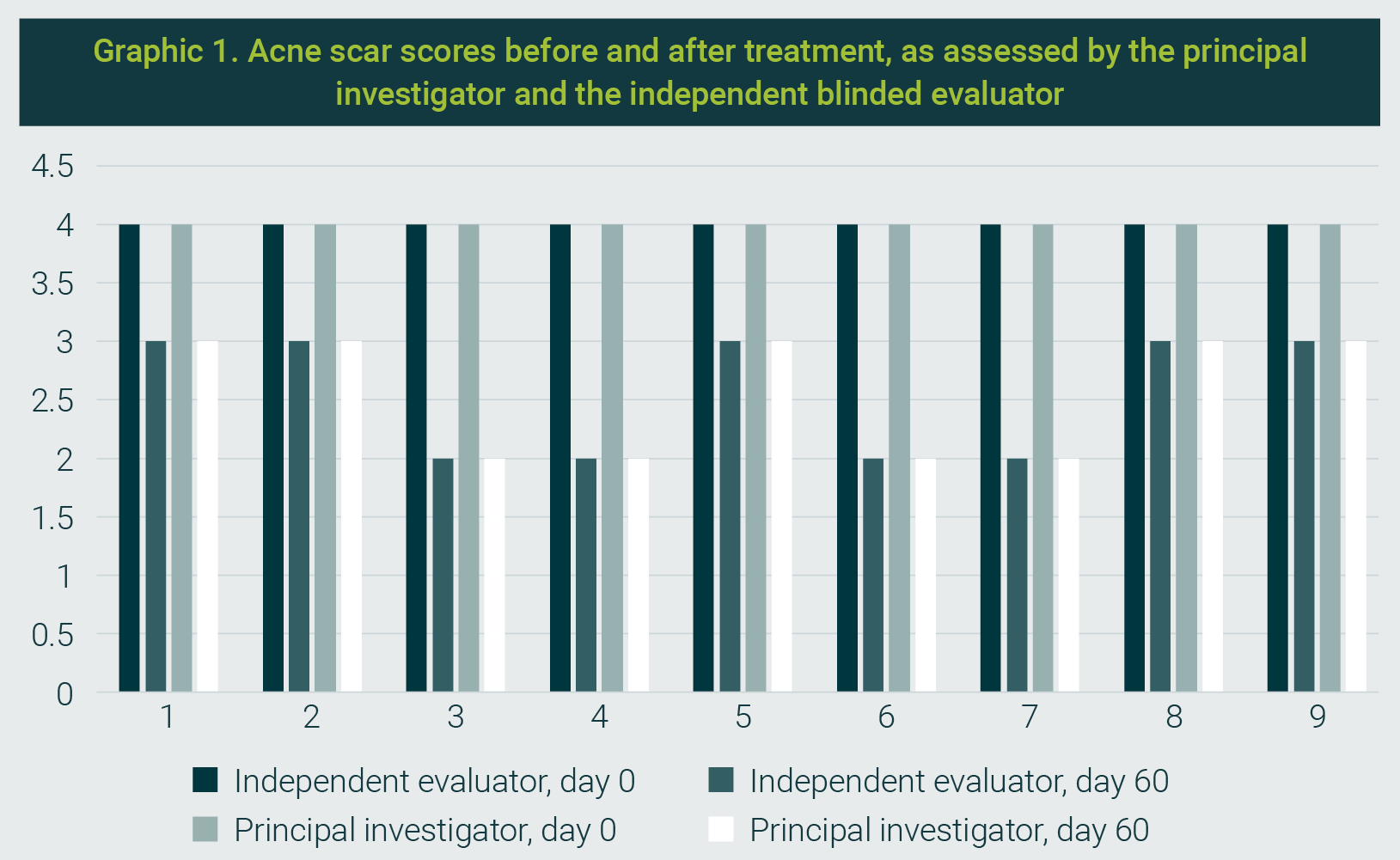
Downloads: 3
Background. Acne scars significantly affect people's quality of life and are classified as atrophic, hypertrophic, or keloid. The use of hybrid cooperative complexes of hyaluronic acid has shown promising results in improving atrophic acne scars by activating fibroblasts and stimulating collagen production. Objective. To evaluate the clinical efficacy and safety of Profhilo® using a dual-plane injection technique for the treatment of atrophic acne scars in a Mexican population. Materials and Methods. A retrospective, multicenter pilot study was conducted involving nine participants who had a Goodman and Baron scores ≥2. Treatments were administered in two sessions (T0 and T1, 30 days apart). Outcomes were assessed at 60 days (T2). The dual-plane injection technique included subcision followed by linear retrograde administration of Profhilo®. Outcomes were measured using the Goodman and Baron Scarring Grading System and a 6-point Likert scale for scar improvement. Patient satisfaction was assessed using the Global Aesthetic Improvement Scale (GAIS). Adverse events were monitored. Results. The study included five men and four women (mean age: 35.3 years). The mean Goodman and Baron score improved from 4.0 at baseline to 2.25 at T2. All patients showed improvement in scar appearance, with most reporting over 50% improvement on the Likert scale. No significant adverse events were reported. Conclusions. The use of Profhilo® with a dual-plane injection technique appears to be a safe and effective option for improving the appearance of atrophic acne scars, resulting in a significant reduction in scar severity and high patient satisfaction.
Introducción. Las cicatrices de acné afectan considerablemente la calidad de vida de las personas; y se les clasifica como atróficas, hipertróficas o queloides. El uso de complejos cooperativos híbridos de ácido hialurónico ha mostrado resultados prometedores para disminuir las cicatrices de acné atróficas mediante la activación de fibroblastos y la estimulación de producción de colágeno. Objetivo. Evaluar la eficacia clínica y seguridad de Profhilo® mediante el uso de la técnica de inyección de doble plano para el tratamiento de cicatrices de acné atróficas en una población mexicana. Material y métodos. Se llevó a cabo un estudio piloto, multicéntrico y retrospectivo, en el que se incluyeron nueve participantes que tenían escalas ≥2 de Goodman y Baron. Los tratamientos se administraron en dos sesiones (T0 y T1, 30 días de separación entre estas dos sesiones). Los resultados finales se evaluaron a los 60 días (T2). La técnica de inyección de doble plano incluyó una subcisión, seguida de la administración retrógrada lineal de Profhilo®. Los resultados se midieron con el sistema de escalas Goodman and Baron Scarring y con la escala de seis puntos Likert para evaluar las mejorías. Los pacientes evaluaron la satisfacción con la escala Global Aesthetic Improvement Scale (GAIS). Se evaluaron los eventos adversos. Resultados. El estudio incluyó cinco hombres y cuatro mujeres (mediana de edad de 35.3 años). La mediana de la escala Good and Baron mejoró desde los valores de referencia de 4.0 a 2.25 en T2. Todos los pacientes mostraron mejoría en la apariencia de las cicatrices; la mayoría de ellos indicó más del 50% de mejoría en la escala Likert. No se registraron eventos adversos significativos. Conclusiones. El uso de Profhilo® con la técnica de inyección de doble plano parece ser una alternativa segura y efectiva para mejorar la apariencia de las cicatrices atróficas de acné, lo cual se traduce en reducción significativa de su severidad y en alta satisfacción de los pacientes.
Acne scars are the result of the resolution of inflammatory lesions (papules, pustules, and nodules) and non-inflammatory lesions (comedones). They are classified as atrophic, hypertrophic, or keloid.
It is estimated that acne scars affect approximately 95% of individuals, significantly impacting their quality of life.1-3
Atrophic scars result from collagen loss following inflammation of the pilosebaceous unit4 and, according to the classification by Jacob et al, are categorized into rolling, boxcar, and icepick scars.5
There are multiple therapeutic alternatives for improving the appearance of atrophic acne scars, including dermal fillers with hyaluronic acid (HA), poly-L-lactic acid, and calcium hydroxyapatite, as well as subcision, punch excision, chemical peels, microneedling, dermabrasion, and laser therapy, among others.6 Most treatments aim to break fibrotic bands beneath the scars and induce new collagen and connective tissue formation.
The combination of high- and low-molecular-weight ultrapure hyaluronic acid—known as hybrid cooperative complexes (HCCs)—has shown significant efficacy in activating fibroblasts and reducing the appearance of acne scars.7 These complexes create a space that prevents reattachment of fibrotic strands in the dermis and encourages new connective tissue formation above the product application, leading to aesthetic improvement.8,9
During wound healing, the hygroscopic properties of hyaluronic acid support hydration and the structural integrity of the extracellular matrix, promoting cell migration, adhesion, and proliferation within granulation tissue.
HA also plays a role in reorganizing the extracellular matrix, collagen deposition, cytokine binding, and the recruitment of matrix metalloproteinases. Therefore, exogenous HA supplementation may benefit the management of aberrant scarring.
Profhilo is a high- and low-molecular-weight HA formulation based on HCCs, developed using patented NAHYCO Hybrid Technology. It is produced by thermally stabilizing a blend of high (1100-1400 kDa) and low (80-100 kDa) molecular weight HA, without the use of chemical crosslinkers like BDDE. The resulting hybrid complexes offer high HA concentration (64 mg/2 mL), low viscosity, high tissue diffusion, and minimal inflammatory response.
An essential feature of HCCs is their ability to integrate into tissue, due to their high cohesivity. They distribute uniformly across anatomical units and exhibit fluidity rather than elasticity—unlike crosslinked HA gels.9
The objective of this study was to retrospectively evaluate a pilot series of patients with atrophic acne scars treated identically with HCCs using a dual-plane injection technique in a Mexican population, in order to assess clinical evolution and improvement.
This was a retrospective, multicenter pilot study involving nine volunteer patients with post-acne scars graded ≥2 according to the Goodman and Baron qualitative global acne scar grading system (Table 1).
| Table 1. Post-acne scars, qualitative global scarring grading system (Goodman and Baron) | ||
|---|---|---|
| Grade | Severity Level | Characteristics |
| I | Macular | These scars are erythematous, hyperpigmented, or hypopigmented macules. They represent a color issue rather than contour irregularities. |
| II | Mild | Mild atrophic or hypertrophic scars that may not be evident from social distances of 0.5 m or more and can be easily covered with makeup or natural hair shadow. |
| III | Moderate | Moderate atrophic or hypertrophic scars that are visible at social distances of 0.5 m or more and are not easily covered; may flatten on manual skin stretching (if atrophic). |
| IV | Severe | Severe atrophic or hypertrophic scars are evident from distances greater than 0.5 m, are not easily covered, and do not flatten upon skin stretching. |
Treatments were administered at private dermatology clinics in Mexico by trained physicians, following a standardized technique.
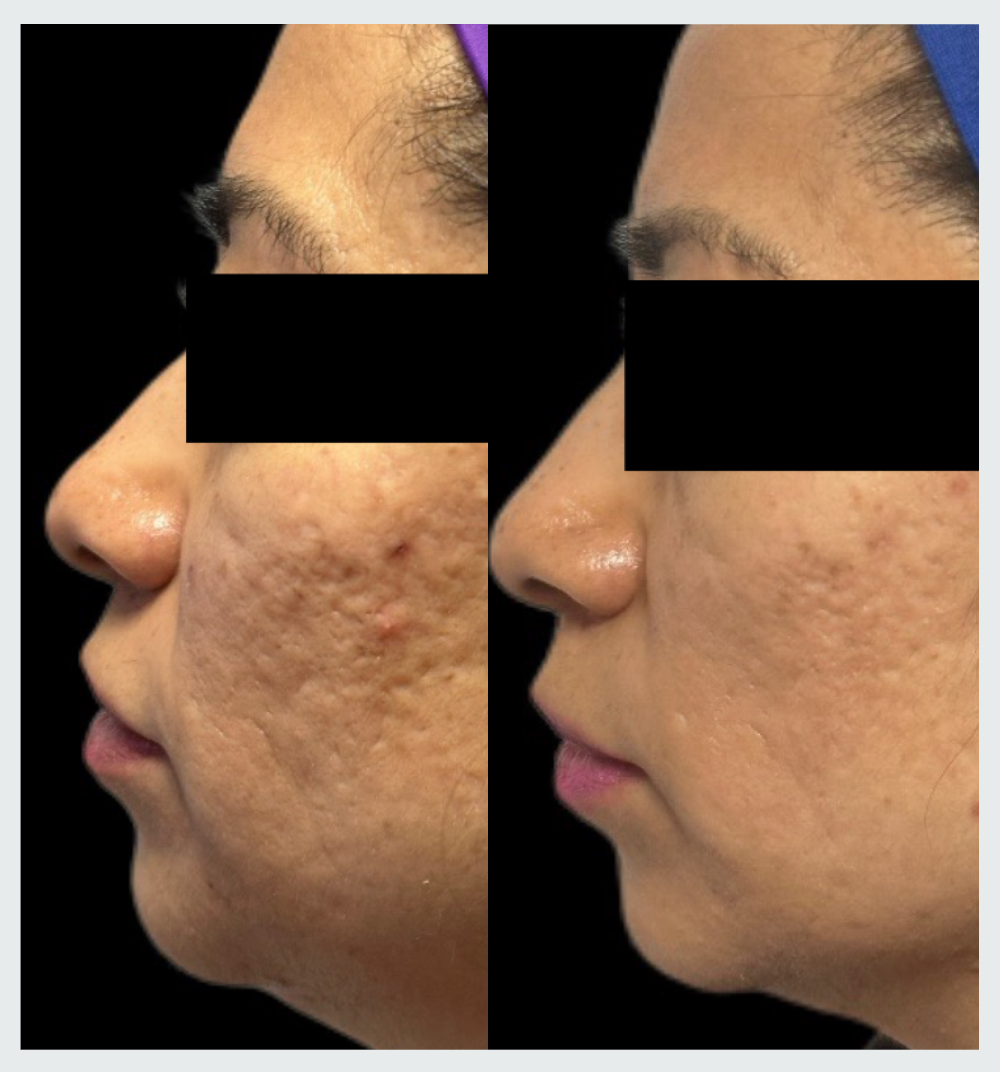
The first treatment was administered at baseline (T0), the second after 30 days (T1), and the final evaluation was at 60 days (T2). Standardized photographs (frontal, oblique, and profile) were taken using a Canon EOS Rebel T7 digital camera at each time point (T0, T1, T2).
The principal investigator assessed scar severity using the Goodman and Baron scale at T0, T1, and T2. The final results were also evaluated by a blinded, independent physician using clinical images from T0 and T2.
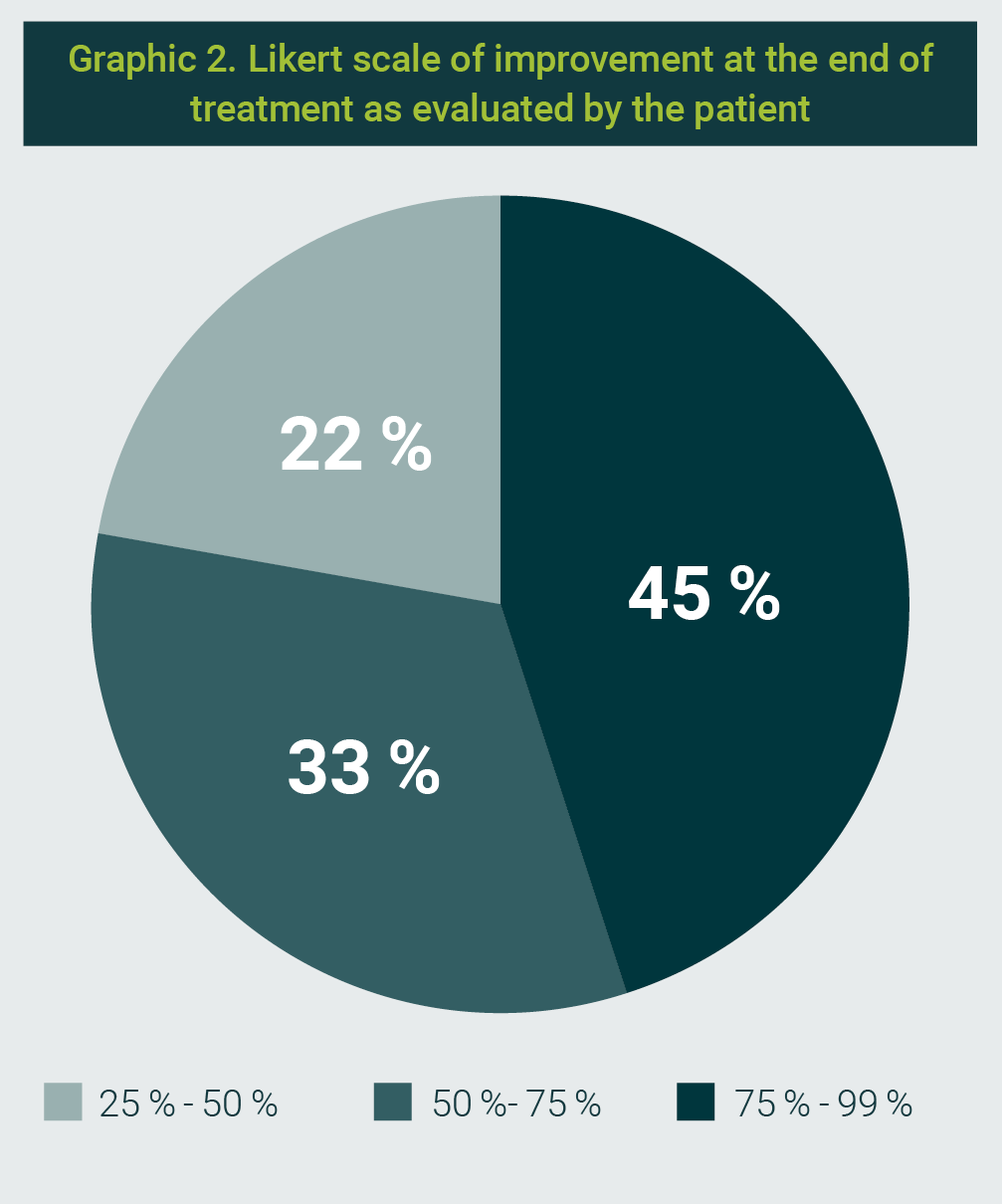
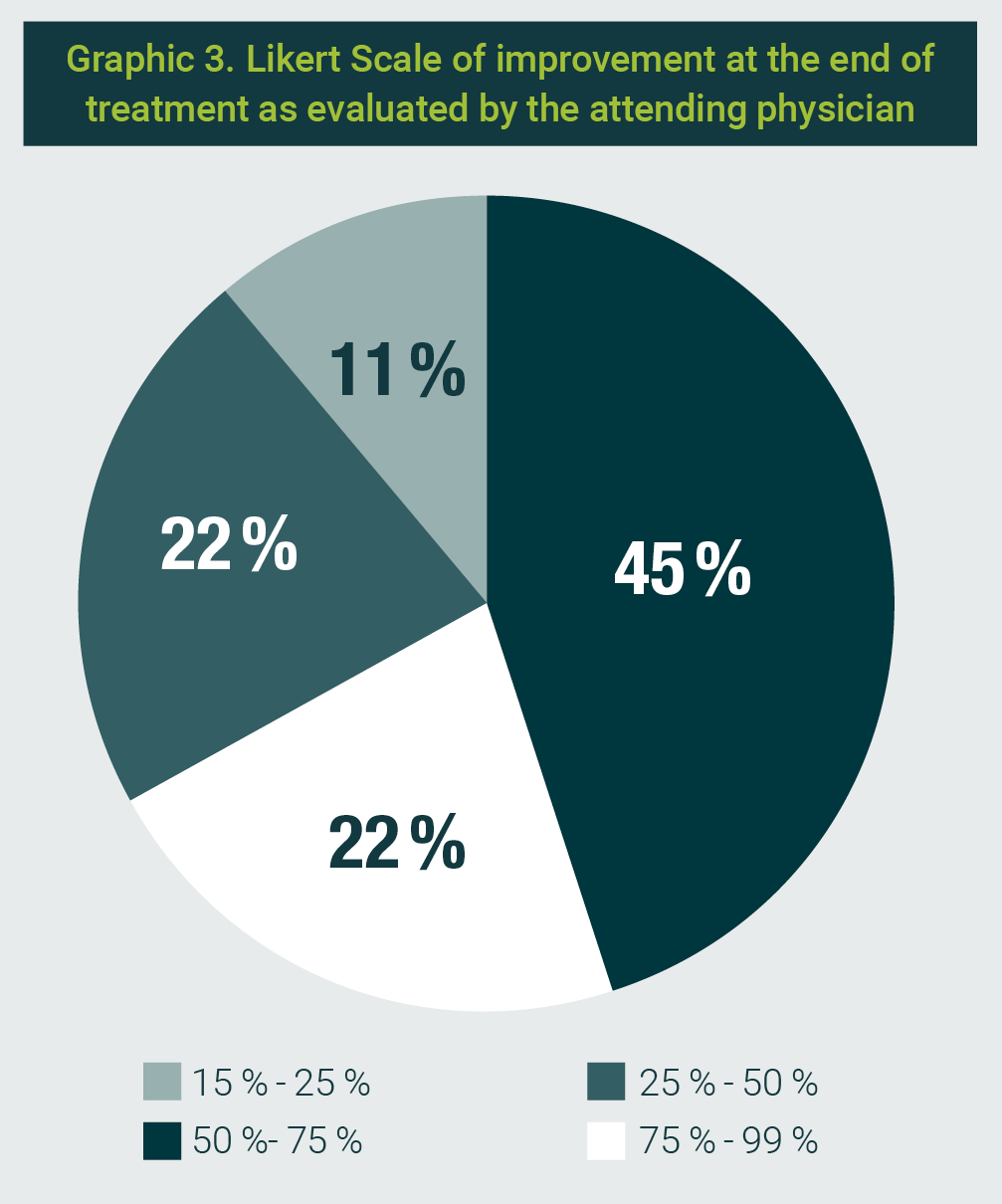
Both treating physicians and patients rated aesthetic improvement at T2 using a 6-point Likert scale: -1: worsening of acne scars; 0: no change; 1: 1-25% improvement; 2: 25-50% improvement; 3: 50-75% improvement; 4: 75-99% improvement.
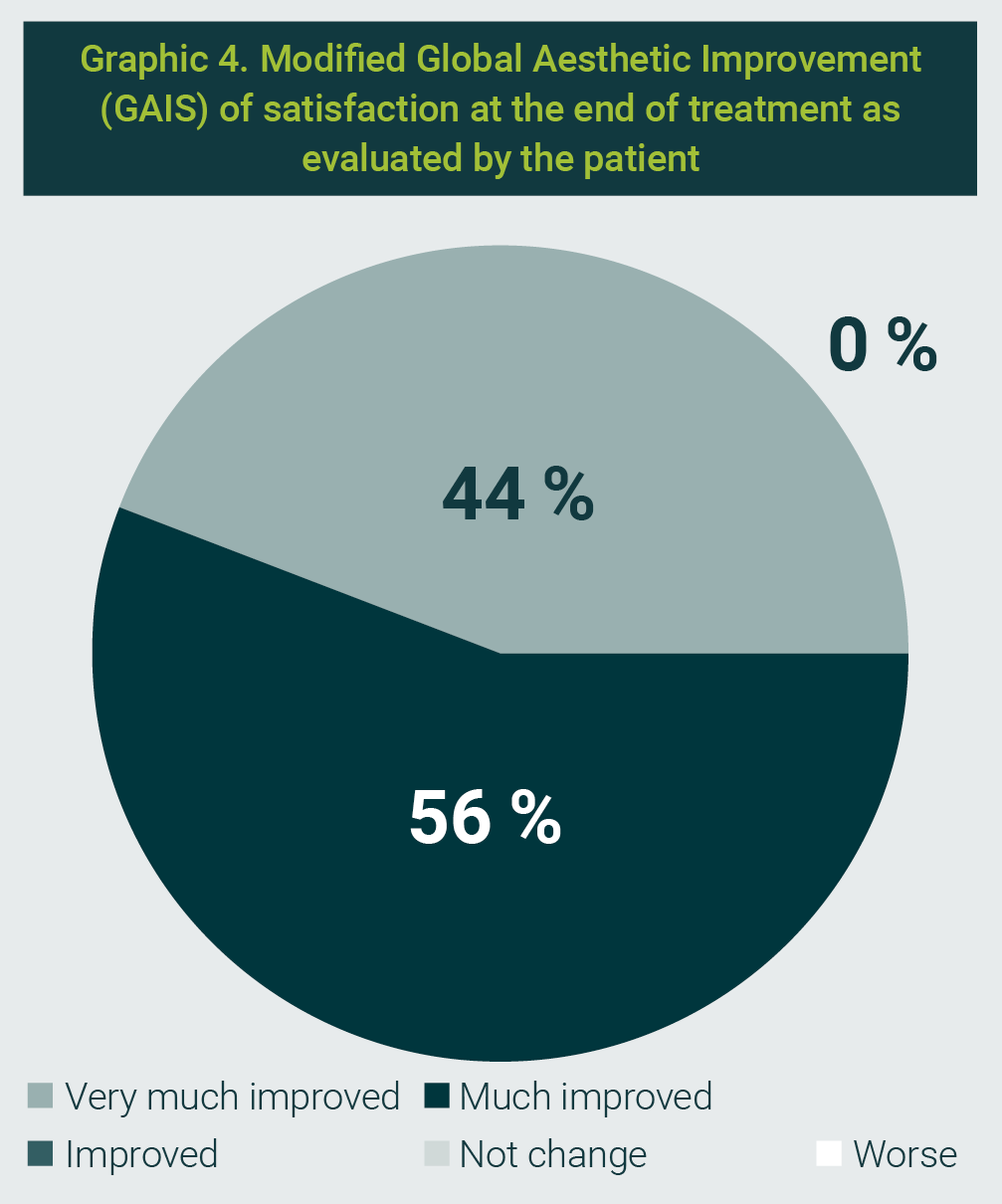
Patient satisfaction was measured at T2 using the 5-point Global Aesthetic Improvement Scale (GAIS): 1 = much improved; 2 = very improved; 3 = improved; 4 = no change; 5 = worse. Adverse events were documented at each visit (T0 and T2).
Inclusion criteria: adults >18 years with rolling, boxcar, or icepick facial scars; Goodman and Baron score ≥2; Fitzpatrick skin types III-IV.
Exclusion criteria: age <18, history of keloids, active inflammatory acne, scars outside the face, previous treatments (injectables, peels, lasers, biostimulators) within 6 months, immunosuppression, active infections (e.g., herpes), isotretinoin therapy, or facial plastic surgery within 12 months.
All patients signed informed consent and completed medical history forms. The study was conducted across multiple private clinics in Mexico by different physicians following standardized protocols.
Before treatment, the face was cleansed with dermo-cleansing foam, and topical anesthetic cream (5% lidocaine, EMLA®; AstraZeneca®) was applied 20 minutes before injection. Aseptic preparation was performed, and patients were placed in a 45° semi-Fowler position.
The injection protocol involved dividing the scarred area into 4x4 cm quadrants, injecting 0.01-0.2 mL of Profhilo® per lesion, depending on severity, using a 29 Gx13mm needle into the deep dermis.
Then, a subdermal application was performed using a 23Gx50mm cannula with subcision and a linear retrograde technique, delivering 0.1-0.2 mL per vector. The same procedure was repeated at T1. After each session, patients were instructed to use only daily sunscreen.
Nine patients were recruited between March and November 2024, including five men and four women. The mean age was 35.3 years.
All patients entered the study with a Goodman and Baron score of 4 and completed it with an average score of 2.25, as evaluated by the principal investigator (Graphic 1).
At the end of treatment, all patients rated the outcome as positive, with improvement greater than 25%, and the majority (45%) rated their improvement as greater than 75% (Graphic 2).
At the end of the treatment, the attending physicians also rated the outcome as positive, with an improvement greater than 15%. In 22% of cases, the result was rated as greater than 75% (Graphic 3).
The GAIS scale for treatment satisfaction at the end of the study was rated by patients within the range of Much improved to Very much improved (Graphic 4).
A clinical photograph showing the before-and-after results of the treatment is presented in Photograph 1. No adverse events were reported.
The treatment of acne scars represents a clinical challenge due to the complex factors that contribute to their formation and persistence. In this study, a dual-plane injection technique was employed with Profhilo®, a hyaluronic acid-based complex, yielding significant reductions in the severity of atrophic scars. The observed outcomes reflect the unique ability of HCCs to activate fibroblasts and stimulate collagen production, thereby promoting dermal regeneration and enhancing the overall appearance of scars.
Compared to other acne scar treatments—such as chemical peels, laser therapies, and other dermal fillers—, the HCC-based approach offers specific advantages:
- low viscosity,
- high tissue diffusion,
- and minimal inflammatory response.
The dual-plane technique effectively targets both the dermal surface and deeper layers, achieving better product integration and preventing the reattachment of scar fibers.
It is well established that HCCs of hyaluronic acid exhibit longer-lasting, fully reversible effects, with high biocompatibility and minimal immunogenicity.
Beyond their dermal effects, HCCs promote adipogenic differentiation and proliferation by upregulating adipogenic genes and associated proteins, leading to tissue bioremodeling across the skin layers. This mechanism is particularly relevant in atrophic acne scars, where subcutaneous fat loss and structural collapse contribute.
In contrast, linear and cross-linked HA formulations primarily exert a volumizing effect, without significantly affecting collagen- or adipocyte-related pathways. Therefore, the observed improvement in fat tissue renewal with HCCs may offer a novel approach to scar correction at deeper planes.
It is important to note that although the results of this study are promising, the relatively small sample size and the absence of a control group limit the generalizability of the findings. Future studies with a randomized, controlled design and larger sample sizes are needed to validate these results and explore long-term efficacy.
Lastly, the standardization of the application technique and the evaluation by an investigator independent from the treating physicians represent a strength of the study, providing reproducible results that can be applied in similar clinical settings.
The treatment of atrophic acne scars with hybrid hyaluronic acid complexes using a dual-plane injection technique proved to be a safe and effective option in the studied population. A significant improvement in scar severity was observed, as measured by the Goodman and Baron scale, along with high patient satisfaction and no significant adverse events.
This approach combines dermal biorevitalization and collagen stimulation, providing an innovative solution for managing atrophic scars. The findings support the implementation of this treatment in daily clinical practice; however, further research is recommended to expand the evidence base and assess its effectiveness across different populations and settings.
We thank the medical and nursing team for their support during the study, as well as the patients for their trust and participation. We acknowledge the academic support from Dermavan | IBSA in training activities. Dermavan | IBSA did not participate in the study design, data analysis, or manuscript preparation.
The authors are speakers for Profhilo®.
| 1. | Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19(4):303-8. |
| 2. | Fabbrocini G, Annunziata MC, D’Arco V, De Vita V, Lodi G, Mauriello MC, et al. Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract. 2010:2010:893080. |
| 3. | Wolfram D, Tzankov A, Pülzl P, Piza-Katzer H. Hypertrophic scars and keloids— A review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009;35(2):171-81. |
| 4. | Clark AK, Saric S, Sivamani RK. Acne scars: How do we grade them? Am J Clin Dermatol. 2018;19(2):139-144. |
| 5. | Jacob CI, Dover JS, Kaminer MS. Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17. |
| 6. | Boen M, Jacob C. A review and update of treatment options using the acne scar classification system. Dermatol Surg. 2019;45(3):411-422. |
| 7. | Avantaggiato A, Girardi A, Palmieri A, Pascali M, Carinci F. Comparison of bio-revitalizing injective products: A study on skin fibroblast cultures. Rejuvenation Res. 2015;18(3):270-276. |
| 8. | Mehrabi J, Shehadeh W, Gallo ES, Artzi O, Horovitz T. Comparison of 2 hyaluronic acid-based fillers for the treatment of acne scars: Structural lifting versus biostimulatory effect. Dermatol Surg. 2023;49(6):581-86 |
| 9. | Cassuto D, Delledonne M, Zaccaria G, Illiano I, Giori AM, Bellia G. Safety assessment of high- and low-molecular-weight hyaluronans (Profhilo®) as derived from worldwide postmarketing data. Biomed Res Int. 2020; 2020:8159047 |
All Rights Reserved® 2019
Latin American Journal of Clinical Sciences and Medical Technology,Publicación contínua • Editor responsable: Gilberto Castañeda Hernández. • Reserva de Derechos al Uso Exclusivo: 04-2019-062013242000-203; ISSN: 2683-2291; ambos otorgados por el Instituto Nacional del Derecho de Autor. • Responsable de la última actualización de este número, Web Master Hunahpú Velázquez Martínez,
Calle Profesor Miguel Serrano #8, Col. Del Valle, Alcaldía Benito Juárez, CP 03100, Ciudad de México, México. Número telefónico: 55 5405 1396 • Fecha de última modificación, 28 de agosto de 2024.
All Rights Reserved® 2019
Publicación contínua • Editor responsable: Gilberto Castañeda Hernández. • Reserva de Derechos al Uso Exclusivo: 04-2019-062013242000-203; ISSN: 2683-2291; ambos otorgados por el Instituto Nacional del Derecho de Autor. • Responsable de la última actualización de este número, Web Master Hunahpú Velázquez Martínez,
Calle Profesor Miguel Serrano #8, Col. Del Valle, Alcaldía Benito Juárez, CP 03100, Ciudad de México, México. Número telefónico: 55 5405 1396 • Fecha de última modificación, 28 de agosto de 2024.